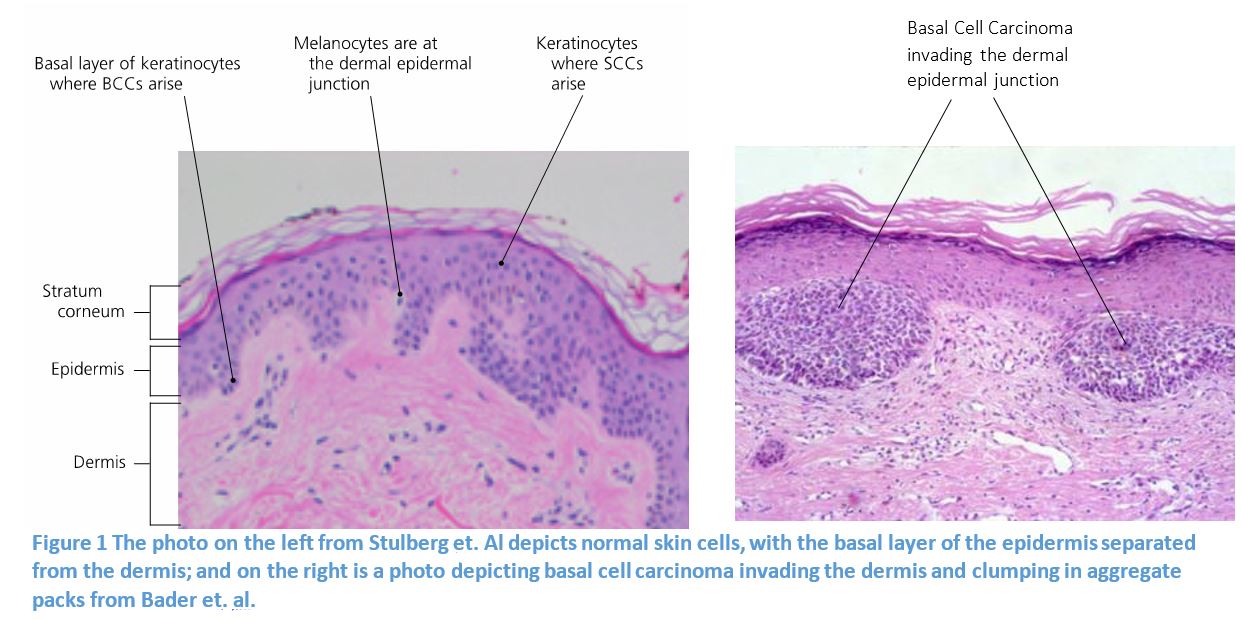
In the United States, skin cancer predominates as the most common form of cancer 3,6. In fact, the rates of skin cancer have doubled from 1982 to 2011 and are projected to continue increasing 3. According to the Skin Cancer Foundation the majority of new skin cancers in 2016 will be basal cell carcinomas (BCC)6. The most superficial layer of skin, the epidermis, contains four layers (5 layers in calloused skin) of continually differentiating keratinocytes2. From the deepest layer, the basal layer, keratinocytes transition through various stages flattening, becoming anucleate, and producing protective keratin2. The basal layer’s function is to provide the next layers of skin to replace the cells that flake off in the most superficial layer2. In figure 1, on the left there is a histology slide of healthy skin; one can see a clear differentiation between the epidermis and dermis, and basal layer is more diffuse. The figure on the right is a histology slide of BCC. The basal layer of cells instead of lying in a flat organized plane, have taken on lobular characteristics and are invading the dermal layer. To the naked eye BCC can be diagnosed as a skin lesion with a central ulcer and a pale border that is increasing in size, raised, poor healing, discolored, waxy or pearly in appearance, painful and itchy10. Once a lesion has been identified and diagnosed as BCC there are multiple options for treatment.
Mohs micrographic surgery (MMS) has the highest cure rate and is the most effective treatment for most types of cancer7, 8. MMS is an outpatient procedure that can be completed the same day, depending on the size of the tumor 5. This method is preferred because it allows for the accurate removal of the tumor, a high cure rate, and preservation of the surrounding skin5. MMS has proven successful in removing larger tumors (greater than 2 cm), infiltrative tumors without clear margins, or a tumor entangled in the nervous or circulatory structures11. The principle behind MMS is identifying all traces of BCC and removing it in order to completely cure the patient4. This involves a layer by layer removal, creating a map of the tumor, and excising any compromised tissue as seen in Figure 2.
An absolute protocol for the timing of reconstruction after tumor removal has not been agreed upon by experts. Some feel immediate reconstruction should be preferred because it will prevent infections, and others feel that delayed reconstruction should be favored due to the time it allows for the confirmation of clean tumor margins thereby preventing recurrence 5. Delayed reconstruction would allow for the surgeon to guarantee that all the BCC has been removed. This guarantee could protect the patient from having to undergo the MMS procedure and reconstruction of the MMS defect again. In a retrospective cohort study using data from two institutions Patel and colleagues sought to uncover the complication rates associated with delayed MMS defect reconstruction. They found the overall complication rate to be 8.2% and the following characteristics to put the patient at risk for a complication: wound larger than 2 cm, exposed bone or cartilage, use of regional flaps with cartilage grafting, reconstruction more than 2 days after the MMS. To overcome the risk of complication due to closure technique, Soliman and colleagues have proposed the use of direct linear closure instead of using local flaps. In a seven year period, at Baylor College of Medicine, 475 of 1354 Mohs defect reconstructions were closed by direct linear repair9. They found that the maximum defect size for direct linear repair was 3.6 cm in the forehead, 3 cm for the lips, 4 cm for the check, and 2.2 cm for the chin9. For very large defects the direct linear repair is not favored, because it may cause a contour deformity, place a lot of tension on the skin, and cause the dog ear effect, skin bunching on one side of a scar9.
Although there are clear and well defined ways to cure BCC there are many preventative measures that can be taken to reduce one’s risk. This includes sun protective behaviors such as using sunscreen and avoiding sunburns 3,6. Melanin in the skin has a role in trying to protect DNA from photo-damage but it is not capable of preventing cancer2,6. Beyond rigorous research, public education on prevention and the signs and symptoms of the early stages of cancer will be critical to reducing the number of people affected by skin cancer.
1..Bader, Robert. “Basal cell Carcinoma Work Up.” Med Scape http://emedicine.medscape.com/article/276624-workup#c8. Date Accessed: 10/19/2016
2..Göppner, D., & Leverkus, M. (2010). Basal cell carcinoma: from the molecular understanding of the pathogenesis to targeted therapy of progressive disease. Journal of skin cancer, 2011.
3..Guy GP, Thomas CC, Thompson T, Watson M, Massetti GM, Richardson LC. Vital signs: Melanoma incidence and mortality trends and projections—United States, 1982–2030. MMWR Morb Mortal Wkly Rep. 2015;64(21):591-596.
4..Mahmoud, B. H. (2016). Overview of Mohs micrographic surgery for the treatment of skin cancers. Journal of the Egyptian Women’s Dermatologic Society, 13(2), 51-54.
5..Patel, S. A., Liu, J. J., Murakami, C. S., Berg, D., Akkina, S. R., & Bhrany, A. D. (2016). Complication Rates in Delayed Reconstruction of the Head and Neck After Mohs Micrographic Surgery. JAMA facial plastic surgery.
6..Reeder, V. J., Gustafson, C. J., Mireku, K., Davis, S. A., Feldman, S. R., & Pearce, D. J. (2015). Trends in mohs surgery from 1995 to 2010: an analysis of nationally representative data. Dermatologic Surgery, 41(3), 397-403.
7..Rowe, D. E., Carroll, R. J., & DAY, C. L. (1989). Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma. The Journal of dermatologic surgery and oncology, 15(4), 424-431.
8..Smeets, N. W. J., Kuijpers, D. I. M., Nelemans, P., Ostertag, J. U., Verhaegh, M. E. J. M., Krekels, G. A. M., & Neumann, H. A. M. (2004). Mohs’ micrographic surgery for treatment of basal cell carcinoma of the face——results of a retrospective study and review of the literature. British journal of dermatology, 151(1), 141-147.
9..Soliman, S., Hatef, D. A., Hollier Jr, L. H., & Thornton, J. F. (2011). The rationale for direct linear closure of facial Mohs’ defects. Plastic and reconstructive surgery, 127(1), 142-149.
10..Stulberg, D. L., Crandell, B., & Fawcett, R. S. (2004). Diagnosis and treatment of basal cell and squamous cell carcinomas. American family physician, 70(8), 1481-1488.
11..Telfer, N. R., Colver, G. B., & Morton, C. A. (2008). Guidelines for the management of basal cell carcinoma. British Journal of Dermatology, 159(1), 35-48.