Last week Dr. John Kim was the University of Toronto keynote lecturer at the 17th annual Toronto Breast Symposium. This internationally attended conference includes lectures, video presentations, open panel discussions, as well as question and answer sessions. The symposium included four major topics: refinements in breast augmentation, autogeneous breast reconstruction, alloplastic breast reconstruction, risk management and complications. Dr. Kim’s presentations were titled: “Risk and Breast Reconstruction: Application of the BRAscore,” “An Al gorithmic Approach to Using ADM in Breast Reconstruction,” and “Shaped versus Round Implants in Breast Reconstruction.” Dr. Kim also participated on a panel discussing the pros and cons of pedicled versus free flap breast reconstruction with other distinguished surgeons Mithcell Brown (Founder of Toronto Annual Breast Surgery Symposium, University of Toronto), John Semple (Women’s College Hospital), Joan Lipa (Sunnybrook Health Sciences Center), Toni Zhong (University of Toronto), and Steven Jacobson (Jacobson Plastic Surgery).
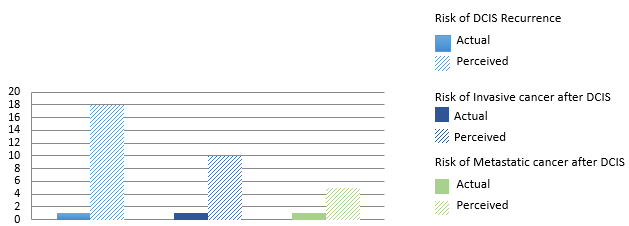
In Dr. Kim’s keynote lecture about risk and breast reconstruction; he discussed the benefits of incorporating risk data into the surgical decision making process to improve outcomes, the appropriate uses of big data, and the perception (or misperception) of risk. One aspect of the presentation discussed how understanding and assessing risk is a very useful means for surgeons to discuss a plan with a patient. Although, Dr. Kim also addresses the issue of a misperception of risk. In a study published in the Journal of the National Cancer Institute, the researchers found that patients had a gross overestimation of their risk. These patient’s all had Ductal Carcinoma in Situ, and after their treatment they were asked what they thought their risk was of: DCIS recurrence, being diagnosed with an invasive cancer, or being diagnosed with metastatic cancer. A way to circumvent this issue is to compare the risk of a medical event to that of a more palatable real world experience. For example, the risk of DCIS recurrence in one of these patients is comparable to the risk of dying in a car accident in one’s lifetime.
In the algorithm presentation Dr. Kim discussed the points surgeons should consider when planning on using ADM: mastectomy and reconstructive technique, BMI, breast size, preoperative radiation, pectoralis anatomy, flap vascularity, and individual patient factors. These considerations can be divided into pre-operative and intra-operative considerations. During his talk he addressed each of these considerations; to learn more about this research click here to see the research Dr. Kim and his research team published on the subject.
His final talk titled, “Using Round v. Shaped Implants in Breast Reconstruction” discussed the current controversies surrounding these implants as well as the pros and cons of either device. When choosing breast implants the questions to consider include: what are my risks of a complication, how likely will I need a reoperation and when, and how will it look. Throughout Dr. Kim’s talk he addresses all of these concerns through examples from his own clinical practice and studied published in peer reviewed journals. To summarize shaped implants have: an anatomic shape which suggests a better aesthetic result, reduced risk of capsular contracture, less likely to rupture, but it has the concern of the textured surface and the possible complications associated with that. Round implants appear to have a lower aesthetic result in some studies (but other studies have shown no difference), a higher risk of capsular contracture, less likely to develop a biofilm on the surface, and will have more natural movement.

1. Jordan SW, Khavanin N, Fine NA, Kim JYS. An algorithmic approach for selective ADM use in immediate two-stage breast reconstruction: Indications and outcomes. Plast Reconstr Surg. 2014;134(2):178-88.
2. Partridge, A., Adloff, K., Blood, E., Dees, E. C., Kaelin, C., Golshan, M., … & Winer, E. (2008). Risk perceptions and psychosocial outcomes of women with ductal carcinoma in situ: longitudinal results from a cohort study. Journal of the National Cancer Institute, 100(4), 243-251.